Five people who had life-altering, seemingly irreversible cognitive deficits following moderate to severe traumatic brain injuries showed substantial improvements in their cognition and quality of life after receiving an experimental form of deep brain stimulation (DBS) in a phase 1 clinical trial. The trial, reported Dec. 4 in Nature Medicine, was led by investigators at Weill Cornell Medicine, Stanford University, the Cleveland Clinic, Harvard Medical School and the University of Utah.
The findings pave the way for larger clinical trials of the DBS technique and offer hope that cognitive deficits associated with disability following traumatic brain injury (TBI) may be treatable, even many years after the injury.
The DBS stimulation, administered for 12 hours a day, targeted a brain region called the thalamus. After three months of treatment, all the participants scored higher on a standard test of executive function that involves mental control, with the improvements ranging from 15 to 55 percent.
The participants also markedly improved on secondary measures of attention and other executive functions. Several of the participants and their family members reported substantial quality of life gains, including improvements in the ability to work and to participate in social activities, according to a report describing participant and family perspectives from the trial. Dr. Joseph Fins, the E. William Davis, Jr., MD Professor of Medical Ethics at Weill Cornell Medicine, led that research effort.
“The ability to keep your focus and ignore the other things that aren’t important to focus on is very, very important to a lot of things in life,” one participant said in the report. “You never know what a blessing it is until you get it the second time.”
“These participants had experienced brain injury years to decades before, and it was thought that whatever recovery process was possible had already played out, so we were surprised and pleased to see how much they improved,” said study co-senior author Dr. Nicholas Schiff, the Jerold B. Katz Professor of Neurology and Neuroscience in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine.
Our aim now is to expand this trial, to confirm the effectiveness of our DBS technique, and to see how broadly it can be applied to TBI patients with chronic cognitive deficits.”
Dr. Jaimie Henderson, study co-senior author, the John and Jene Blume – Robert and Ruth Halperin Professor in the Department of Neurosurgery at Stanford University School of Medicine
A cognitive pacemaker?
Recent estimates by the Centers for Disease Control & Prevention suggest that in the United States alone, TBI accounts for more than 200,000 hospitalizations and more than 60,000 deaths annually, with roughly five million Americans suffering from long-term, TBI-related cognitive disability.
This chronic disability typically involves memory, attention and other cognitive deficits along with related personality changes, which together impair the individuals’ social relationships, ability to work and overall ability to function independently. Traditionally, researchers have assumed that these problems stem from irreversible brain-cell loss and are thus untreatable.
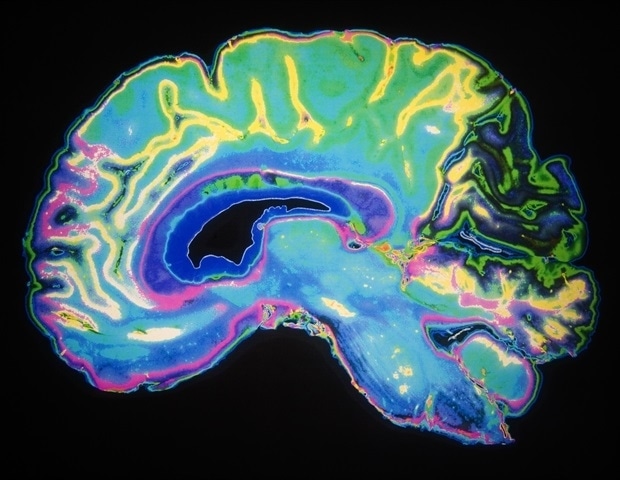
However, Dr. Schiff’s work has shown that activity in a specific brain circuit, which the investigators termed the ‘mesocircuit,’ underlies deficits in attention, planning and other abilities known as executive cognitive functions, after TBI, and that such functions may be at least partially recoverable. A brain region called the central thalamus normally serves as a kind of energy regulator for this cognitive circuit. Though this region is generally damaged by a TBI, stimulating it via DBS may restore its activity, and thus reactivate the cognitive circuits it serves.
“Basically, our idea has been to overdrive this part of the thalamus to restore brain function, much as a cardiac pacemaker works to restore heart function,” Dr. Schiff said.
In a 2007 study, Dr. Schiff and colleagues showed that DBS targeting the central thalamus markedly improved measures of cognition and behavior in a person with severe TBI who had been in a minimally conscious state for six years. That success, and related preclinical research, led to the new study.
“Every day is a battle”
The participants in the new study, four men and one woman, had regained independence in daily function, but cognitive deficits involving executive functions, stemming from TBIs three to 18 years prior, prevented return to pre-injury levels of work, academic study and social activities.
“Every day is a battle, although I try and be upbeat,” one male participant told the researchers in an interview conducted prior to the treatment. “[I]t’s not the quality of life I really want to live. And so, I’m willing to take the chance, to even get—if I can even get five or 10 percent better . . .”
“Despite decades of costly research, we have barely moved the needle in preventing or reducing TBI-related disability. Our results, although preliminary, suggest that DBS may improve cognitive function well into the chronic phase of recovery,” said Dr. Joseph Giacino, a neuropsychologist who helped design the trial, and served as co-first author of the 2007 study. Dr. Giacino is the director of rehabilitation neuropsychology at Spaulding Rehabilitation Hospital, a staff neuropsychologist at Massachusetts General Hospital and a professor in the Department of Physical Medicine and Rehabilitation at Harvard Medical School.
The surgery
Dr. Henderson and his surgical team implanted each subject with DBS electrodes positioned to stimulate a part of the thalamus called the central lateral (CL) thalamic nucleus, along with an associated bundle of nerve fibers.
The implantation was guided by brain imaging (MRI and CT) of each subject. One type of MRI was processed with a novel algorithm developed by Dr. Brian Rutt’s group at Stanford to provide high-resolution outlines of CL and other relevant thalamic nuclei, which were then combined with 3D maps of nerve fiber tracts passing through these nuclei. Computer models of how DBS electrodes would interact with CL neurons and nerve fibers were developed by biomedical engineer Dr. Christopher Butson and colleagues, who were at the University of Utah during the study.
“Participant-specific models were used to create pre-operative surgical plans and guide post-surgical DBS programming to maximize activation of CL brain circuits while minimizing activation of surrounding thalamic circuits,” said Dr. Butson, now the Endowed Chair of Neurotherapeutics at the Fixel Institute. “Using this approach, we were able to focus stimulation in areas that had the highest likelihood of improving executive function.”
Neurosurgeon Dr. Andre Machado, chairman of the Neurological Institute at Cleveland Clinic, who previously worked with Dr. Schiff on DBS studies of minimally conscious participants, also helped develop the surgical procedure in the new study.
“Targeting very specific parts of the brain after a devastating injury is complex, as each person is affected in different ways by the trauma,” said Dr. Machado. “The success of this study is the fruit of multi-institutional, professional collaboration and the combination of many teams to address a gap in healthcare. This is how good science happens.”
In each participant, the wires coming from the thalamus-stimulating electrodes were placed beneath the skin, running to a battery pack and controller implanted in the upper chest—again, like a cardiac pacemaker.
Trial meets safety and efficacy goals
Starting two to three months after implantation surgery, the study team tested the DBS in each participant, fine-tuning the stimulation signal and checking for side effects.
Prior to this initial testing period, one of the original six participants experienced a scalp infection, had her DBS electrodes removed, and was withdrawn from the study. But the other five experienced minor or no side effects from the surgery or the DBS stimulation.
“At this point, I’m comfortable saying that this thalamic target is really quite benign in terms of side effects from the stimulation,” Dr. Henderson said.
Following the fine-tuning and safety-check period, the five participants were treated by DBS for twelve hours a day, the signals being switched off at night. The primary measure of efficacy was the change in the participant’s score, from before surgery to after the 90-day treatment window, on a standard executive function test called the trail-making test part B (TMT-B). The researchers’ pre-set threshold for a clinically meaningful improvement was a 10 percent increase in the TMT-B score.
As it turned out, every one of the five participants exceeded that threshold. While perceived and measured efficacy of the treatment varied, some participants and their families reported life-changing results. One mother told the investigators in the post-treatment report, “I got my daughter back… It’s a miracle. It’s so profound for us.”
Even now, several years after the study was completed, all five participants still have their DBS implants, some with new batteries, Dr. Henderson said.
Looking ahead
To the researchers, the findings indicate that thalamus-targeted DBS has the potential to meaningfully boost cognitive function and quality of life for many people with moderate to severe TBI.
They now plan a phase 2 clinical trial, with 25 to 50 participants, to optimize the treatment, to confirm its safety and efficacy and to understand better the type of patient with TBI that is best suited for it. If that trial goes well, a larger and more conclusive, phase 3 study would follow.
“There’s a long road ahead, but at least we have a road,” Dr. Schiff said.
Source:
Journal reference:
Schiff, N. D., et al. (2023). Thalamic deep brain stimulation in traumatic brain injury: a phase 1, randomized feasibility study. Nature Medicine. doi.org/10.1038/s41591-023-02638-4.