In a recent review published in the journal Neuropsychopharmacology, a group of authors elucidated the intracellular dynamics of antidepressants, challenging the traditional extracellular interaction perspective by exploring their chemical and pharmacological properties and evaluating their subcellular activity and distribution characteristics.
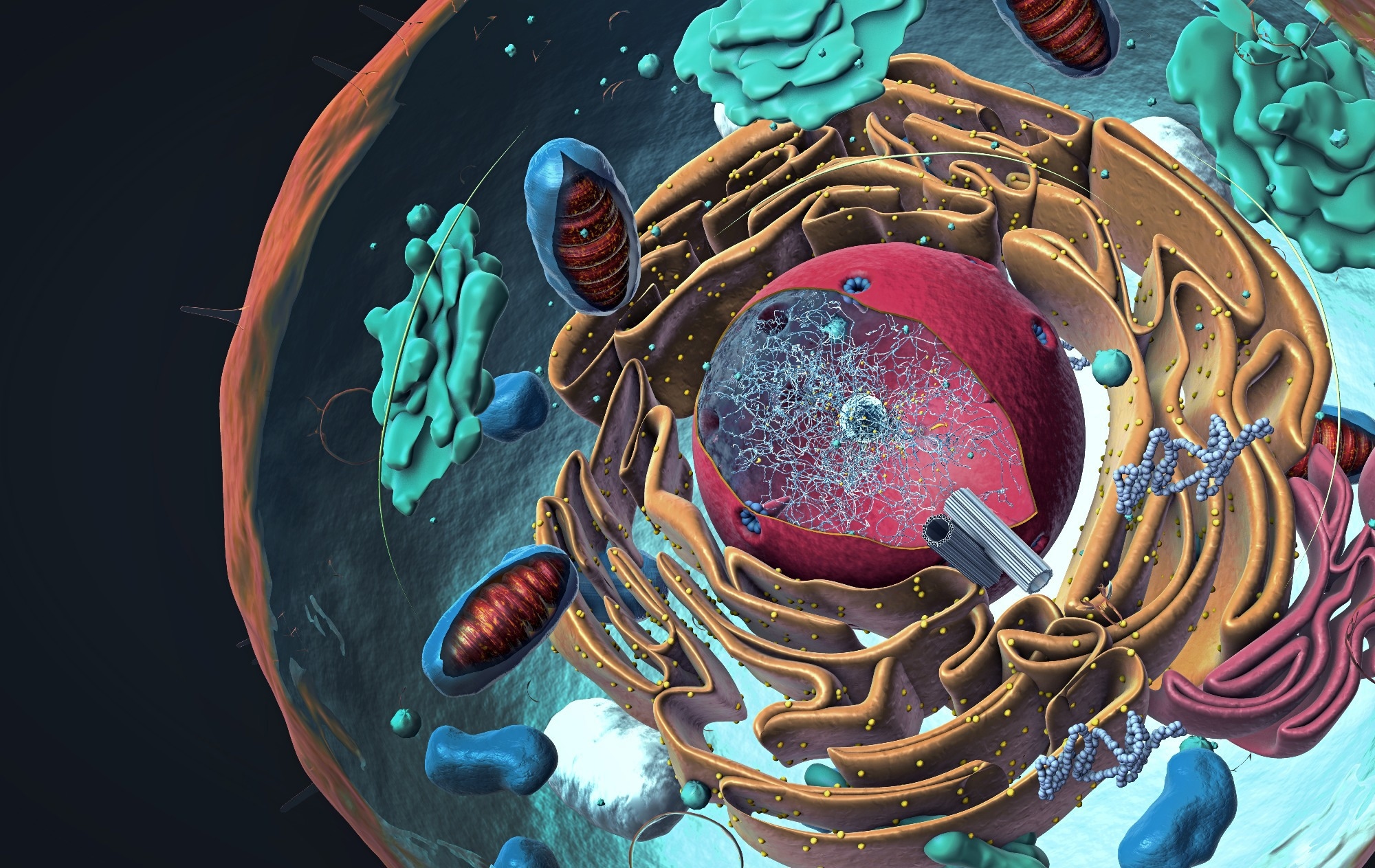
Study: Antidepressants enter cells, organelles, and membranes. Image Credit: Christoph Burgstedt / Shutterstock
Background
Since the early 1900s, neuropharmacological progress has primarily focused on drugs interacting with extracellular plasma membrane targets like ion channels, receptors, and transporters, triggering downstream cellular pathways. Antidepressants, vital but complex agents, span various compounds, from lithium to anesthetics to neurosteroids. The prevailing framework suggests extracellular binding initiates their effects, although precise mechanisms remain elusive. However, evidence shows that several antidepressants interact with intracellular targets. Examples include monoamine oxidase inhibitors targeting mitochondrial enzymes, lithium’s assumed intracellular binding sites, and recent findings on psychedelics and serotonin receptors inside cells. Additionally, certain abused substances exhibit intracellular binding. Further research is crucial as the current understanding of antidepressants is rooted in extracellular binding frameworks. At the same time, emerging evidence points to significant intracellular interactions, necessitating a deeper exploration of intracellular mechanisms and drug permeation principles for comprehensive insight into their therapeutic actions.
Impact of protonation-deprotonation on drug permeation
The permeation of antidepressant drugs across cellular membranes is significantly influenced by their charge status, which is determined by protonation-deprotonation events. The lipid bilayer of cell membranes prefers accommodating uncharged molecules, enabling them to diffuse more easily compared to their charged counterparts. This preference is crucial in the drug’s interaction with target sites within the cell or in organellar lumens.
Key metrics: LogP, pKa, and LogD
Logarithm of the partition coefficient P (LogP), Acid dissociation constant Ka (pKa), and Logarithm of the distribution coefficient (D) at a particular pH (LogD) are crucial for understanding drug permeation through membranes. LogP indicates hydrophilicity or hydrophobicity; pKa reveals a compound’s proton gain or loss propensity at varying pH levels, affecting its charge; LogD, considering charge, predicts drug distribution, especially in the central nervous system (CNS).
Supracellular pharmacokinetics and Lipinski’s rules
Lipinski’s rules, or the “Rule of Five,” are general principles used to predict a drug’s oral bioavailability based on its chemical properties, including LogP (or its more relevant form, LogD at pH 7.4), molecular weight, and hydrogen bond donors and acceptors. While not absolute, these criteria help identify compounds with better potential for absorption and effectiveness when taken orally. However, these rules do not provide insight into a drug’s mechanism of action or potential cytotoxicity.
Emerging insights into subcellular pharmacokinetics
The advent of subcellular drug studies
Despite early hints from Nobel laureates like Mitchell and de Duve, detailed studies on drug dynamics at the subcellular level only gained traction around 2010, thanks to technological advancements. Key methods driving this progress include advanced mass spectrometry and drug-sensing fluorescent reporters, which have revealed significant cellular uptake for drugs like escitalopram and fluoxetine, one of the highest recorded for any substance.
Drug-membrane interactions: Beyond simple metrics
Subcellular volume distribution (Vd) hinges on a drug’s membrane affinity, inadequately reflected by traditional LogD measures. Higher LogD often means increased Vd, influenced more by drug-phospholipid interactions than by LogP or LogD. Isothermal titration calorimetry reveals deeper interaction dynamics with membrane proteins.
Antidepressant interactions with cellular membranes
Antidepressants alter lipid bilayer properties and disrupt cholesterol-rich lipid rafts, affecting cellular signaling and protein distribution. Their affinity for Tyrosine receptor kinase B (TrkB) receptors in these rafts may influence antidepressant effectiveness through cholesterol-dependent mechanisms.
Challenges in Subcellular Drug Targeting
Understanding whether drugs within the plasma membrane (PM) can efficiently reach their targets remains complex. While certain models suggest a membrane approach is unlikely for multidrug transporters, others offer contrasting perspectives based on impermeant drug analogs. For instance, studies with serotonin transporters (SERT) indicate a possible membrane entry route. However, determining the exact mechanism requires further investigation.
Acid trapping and Intracellular drug accumulation
Weak basic drugs are prone to “acid trapping” in organelles like lysosomes, with accumulation influenced by factors like drug pKa, organelle pH, and membrane potential. Drugs around a pKa of 8 are especially susceptible. This non-stereoselective process has significant therapeutic impacts, especially for antipsychotics. However, measuring in-organelle drug concentrations is challenging due to sensor limitations in low-pH conditions. Enhancing these sensors or utilizing alternative fluorophores is vital for unraveling drug dynamics in organelles, potentially uncovering SSRI effects on mitochondrial functions.
Uncharted territory: Drug dynamics in spine synapses and membrane-less organelles
Neuroplasticity and antidepressant action
While neuroplastic changes at spine synapses are believed to be crucial for antidepressants’ effects, direct evidence of these drugs’ accumulation within various synaptic components is scarce. Current tools, such as fluorescent biosensors, have not detected significant localization of Selective Serotonin Reuptake Inhibitors (SSRIs) within these regions.
Membrane-less organelles: The next frontier
Structures like presynaptic release zones and postsynaptic densities devoid of a surrounding membrane present a new challenge. Their unique macromolecular composition likely affects local drug properties, potentially altering pharmacokinetics. However, research on drug interactions within these dense phases is virtually non-existent, marking an exciting direction for future studies.
Ketamine’s pharmacokinetic profile and use in depression treatment
Ketamine, a notable anesthetic and antidepressant, follows Lipinski’s rules but has low bioavailability (24%) due to extensive liver metabolism, affecting brain penetration. Its enantiomers interact differently with N-Methyl-D-Aspartate Receptor (NMDAR), with stereospecific metabolism preserving their chiral centers, offering unique therapeutic potentials.
Administration methods and clinical implications
For clinical use, especially in depression treatment, ketamine’s administration mode is crucial due to varying bioavailability. Intravenous (IV) infusion is common for its quick plasma concentration achievement, yet it’s resource-intensive. Alternative methods like intramuscular (IM) injections and oral intake are available but come with drawbacks like lower bioavailability (oral) and accessibility issues. Intranasal (IN) administration, however, presents a promising balance, offering higher bioavailability (45%) and easier application, partially due to the avoidance of first-pass metabolism. These attributes underpin the Food and Drug Administration’s (FDA’s) 2019 approval of intranasal esketamine for treatment-resistant depression.
Metabolites’ role in ketamine’s antidepressant effects
Investigations into ketamine’s metabolites reveal their prolonged presence in the system post-administration, suggesting their potential contribution to its antidepressant effects. Notably, ketamine is metabolized into hydroxynorketamine (HNK) enantiomers and various dehydroxynorketamine (DHNK) metabolites, all retaining chiral centers. These metabolites, detectable up to three days post-infusion, may offer lower side effect profiles while still combating depressive symptoms. Specifically, (2 R,6 R)-HNK shows promise in rodent studies for its antidepressant-like effects without NMDA receptor interaction, potentially operating through TrkB receptor engagement.
Exploring other rapid-acting antidepressant candidates
Beyond ketamine, other substances like methoxetamine (MXE) and scopolamine are being explored for their antidepressant potential. MXE, similar to ketamine in structure and NMDAR antagonism, shows longer-lasting effects in rodent studies, hinting at its possible utility in depression treatment. Scopolamine, though differing structurally, meets critical drug-likeness criteria but faces challenges in oral bioavailability, potentially limiting its therapeutic application.
Prodrug dynamics in antidepressant and psychedelic compounds
Understanding the role of prodrugs and active metabolites is vital in the pharmacotherapy of depression. For instance, bupropion, an atypical antidepressant, undergoes metabolic conversion to its more active form, hydroxybupropion. Similarly, the psychedelic compound psilocybin is metabolized to psilocin, contributing to its antidepressant properties. Recent studies indicate that these substances may exert their effects through neuroplasticity promotion, likely mediated by TrkB receptor binding, highlighting the complexity and potential of intracellular targets in depression treatment.
Intracellular targeting in neuropsychopharmacology
The field of neuropsychopharmacology is gradually recognizing the importance of intracellular targets in drug development, deviating from the traditional focus on extracellular points of intervention like ion channels and receptors. As research progresses, there’s an anticipatory trend toward an increased number of neuropsychiatric medications interacting with intracellular components, potentially leading to more effective treatment strategies for disorders like depression.